
In recent years, Red Light Therapy (RLT) has emerged as a beacon of hope for enhancing the quality of life for individuals navigating the challenges of cancer. As a complementary therapy, RLT does not aim to treat cancer itself. Instead, it offers a supportive role, focusing on alleviating some of the physical and psychological burdens that come with the disease and its conventional treatments. This article seeks to shed light on how RLT, through its scientifically backed mechanism known as photobiomodulation, can play a pivotal role in improving the well-being of cancer patients.
At its core, RLT involves the use of low-level wavelengths of red light, typically ranging between 630 to 670 nanometers. This therapy capitalizes on the principle of photobiomodulation, a process that stimulates cellular energy production and fosters a healing environment within the body. When exposed to specific wavelengths of red light, mitochondria—the powerhouse of cells—absorb this energy and enhance their function. This leads to an increase in the production of adenosine triphosphate (ATP), the energy currency of the cell, which plays a crucial role in cellular repair, regeneration, and overall energy levels.
The benefits of RLT extend beyond cellular rejuvenation, offering anti-inflammatory effects and contributing to the reduction of oxidative stress within the body. These aspects are particularly relevant for cancer patients, who often face a multitude of side effects from traditional cancer therapies. RLT presents a non-invasive, low-risk option that targets these challenges, aiming to improve patients’ quality of life by addressing issues such as pain, fatigue, and wound healing, without the use of additional medications or invasive procedures.
This article aims to educate potential customers and patients on the scientific foundations and benefits of Red Light Therapy in a supportive cancer care setting. By delving into the biological and technical nuances of RLT’s mechanism of action, we aim to provide a comprehensive understanding of how this therapy can serve as a valuable addition to the holistic care of cancer patients, enhancing their physical well-being and psychological resilience during their journey.
Red Light Therapy Benefits for Cancer Patients
Red Light Therapy (RLT) offers a spectrum of benefits designed to improve the quality of life for cancer patients. Through its non-invasive approach, RLT provides supportive care that addresses several challenges faced by individuals undergoing cancer treatment. Here, we explore the key benefits of RLT, backed by scientific principles and the physiological mechanisms of action, that contribute to the well-being of cancer patients.
IMPROVED WOUND HEALING
Cancer treatments, such as surgery and radiation, can lead to wounds and skin lesions that may heal slowly. RLT accelerates the healing process by stimulating collagen production and enhancing the formation of new blood vessels (angiogenesis). This not only speeds up wound closure but also improves the strength and quality of the healed tissue. The increased ATP production and improved cellular function foster an optimal environment for tissue repair and regeneration.
PAIN MANAGEMENT
Pain is a common symptom experienced by cancer patients, whether due to the disease itself or as a side effect of treatments. RLT’s ability to modulate inflammation and reduce oxidative stress plays a crucial role in its pain-reducing effects. By decreasing inflammation and enhancing blood flow, RLT can alleviate chronic pain, including neuropathic pain, providing a sense of relief without the need for additional medications.
FATIGUE REDUCTION
Cancer-related fatigue is a pervasive issue that significantly impacts patients’ quality of life. RLT combats fatigue by boosting mitochondrial function, leading to increased energy production at the cellular level. This enhancement of ATP availability supports overall energy levels, helping patients feel more vitalized and less burdened by fatigue.
ENHANCED QUALITY OF SLEEP
Sleep disturbances are frequent among cancer patients, with impacts on healing and overall well-being. RLT has been shown to improve sleep patterns and quality by regulating circadian rhythms and reducing pain and anxiety, which can interfere with restful sleep. The calming effect of RLT, coupled with its pain management benefits, contributes to better sleep, which is essential for the body’s recovery processes.
MANAGEMENT OF ORAL MUCOSITIS
Oral mucositis, a painful inflammation and ulceration of the mucous membranes in the mouth, is a common side effect of chemotherapy and radiation therapy. RLT promotes healing and reduces the severity of oral mucositis by enhancing tissue repair, reducing inflammation, and alleviating pain. This can significantly improve patients’ ability to eat and drink, thus maintaining nutrition and hydration, which are critical during cancer treatment
Red Light Therapy emerges as a supportive modality that can significantly enhance the quality of life for cancer patients. By addressing pain, fatigue, wound healing, sleep quality, and the management of oral mucositis, RLT provides a multifaceted approach to supportive care. Its underlying mechanisms—photobiomodulation, anti-inflammatory effects, and enhancement of cellular function—underscore RLT’s role as a beneficial adjunct therapy in the holistic care of cancer patients. As research continues to evolve, the potential of RLT in cancer care underscores the importance of innovative therapies in improving patient outcomes and well-being.
What Is Red Light Therapy?
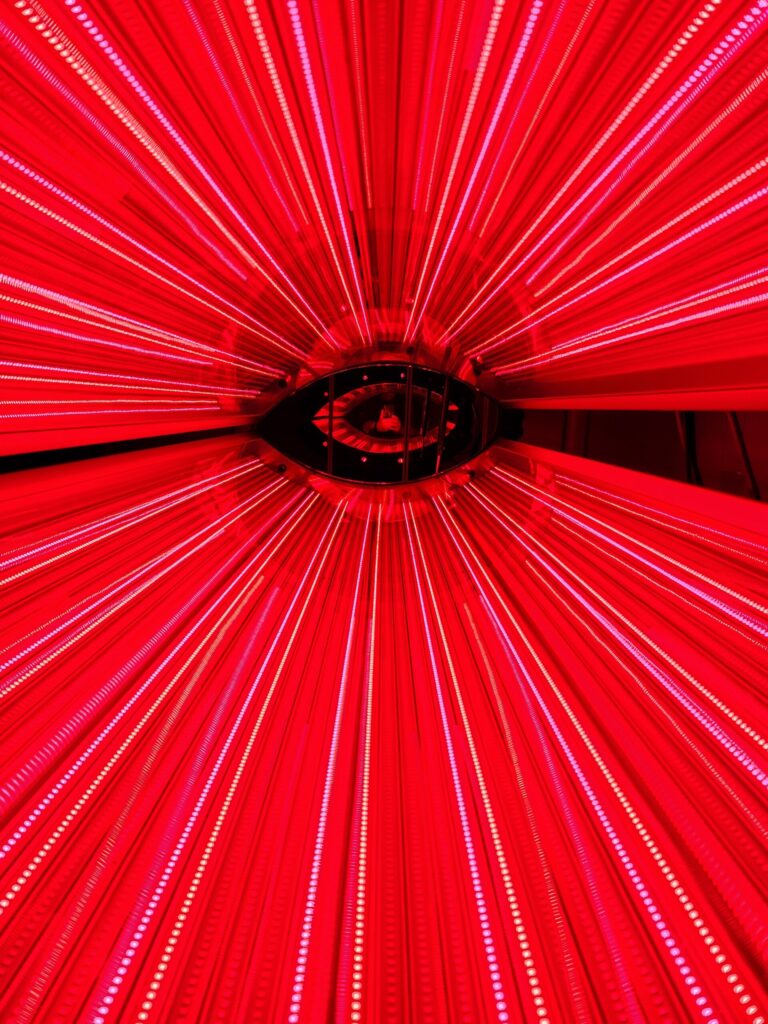
Red Light Therapy (RLT) is a therapeutic technique that harnesses the power of low-level red light wavelengths to initiate biological processes beneficial to health and recovery, especially in the context of supportive cancer care. The therapy operates primarily within the 630 to 670 nanometer range, a spectrum of light that is not only safe for human exposure but also highly effective in penetrating skin and tissue to reach cells in need of rejuvenation.
The cornerstone of RLT’s effectiveness lies in a process known as photobiomodulation (PBM). This process is akin to photosynthesis in plants but occurs within the mitochondria of human cells. The mitochondria are often referred to as the cell’s powerhouse because they produce adenosine triphosphate (ATP), which is vital for energy transfer within cells. When cells are exposed to red light, mitochondria absorb this light and become more efficient at producing ATP. This increase in ATP availability enhances cell function, promotes repair, and encourages the growth of new cells.
Photobiomodulation also leads to a cascade of secondary effects beneficial for health and recovery. For instance, it stimulates the release of nitric oxide, a compound that improves blood flow and reduces oxidative stress. This, in turn, facilitates better oxygen and nutrient delivery to cells, aiding in their recovery and function. Moreover, RLT helps in reducing inflammation by modulating inflammatory pathways, thereby alleviating pain and swelling.
The application of RLT has a rich history, evolving from simple beginnings to a sophisticated therapy backed by scientific research. Initially observed for its potential in accelerating plant growth, the therapeutic effects of red light on human tissue were soon recognized, leading to the exploration of its benefits in various medical contexts. Today, RLT is utilized for a wide range of health-related purposes, including skin health, muscle recovery, and as a complementary therapy in cancer care to improve the quality of life for patients.
In the realm of cancer care, RLT stands out not as a cure but as a supportive therapy aimed at enhancing patient well-being. Its non-invasive nature and the absence of significant side effects make it an appealing option for those seeking to mitigate the physical discomforts associated with cancer and its treatments. By understanding the scientific principles and biological mechanisms underpining RLT, patients and caregivers can better appreciate how this therapy offers a ray of hope in supporting recovery and improving life quality amidst the challenges of cancer.

Clinical Research About Red Light Therapy for Cancer Patients
The exploration of Red Light Therapy (RLT), or photobiomodulation (PBM), in the context of cancer care, has garnered significant attention in recent years. As researchers and clinicians strive to enhance the efficacy and reduce the side effects of cancer therapies, RLT has emerged as a promising adjunctive strategy. Current research and clinical evidence underline the safety, efficacy, and versatility of RLT in managing a broad spectrum of cancer-related complications. This review synthesizes findings from leading studies and position papers, offering insights into the integration of RLT within oncology practices.
EVIDENCE FOR PBM IN CANCER CARE MANAGEMENT
A pivotal position paper titled “Photobiomodulation therapy in management of cancer therapy-induced side effects: WALT position paper 2022” provides a comprehensive overview of RLT’s applicability in oncology. The paper asserts, “There is robust evidence for using PBM to prevent and treat a broad range of complications in cancer care. Specific clinical practice guidelines or evidence-based expert consensus recommendations are provided.”[1] This statement underscores the growing acknowledgment within the scientific community of RLT’s potential to mitigate the adverse effects of cancer treatments. By offering evidence-based guidelines, the paper supports the integration of RLT into clinical practice, highlighting its role in enhancing patient care and outcomes.
SAFETY AND EFFICACY OF PBM IN ONCOLOGY
Further supporting the case for RLT, a systematic review titled “Safety and efficacy of photobiomodulation therapy in oncology: A systematic review” evaluates the therapy’s impact on cancer therapy-related side effects. The review concludes, “PBM (in the red or NIR spectrum by definition) appears safe and successful in the management of cancer therapy‐related side effects. Therefore, PBM should be considered as part of the standard of care for specific oncology purposes.”[2] This statement emphasizes the therapy’s safety profile and its success in alleviating side effects, advocating for its adoption as a standard care component in oncology.
Research spanning various types of cancer and treatment modalities has demonstrated RLT’s effectiveness in reducing side effects such as oral mucositis, dermatitis, lymphedema, and neuropathy. Clinical trials have reported significant improvements in pain management, wound healing, and overall quality of life for patients undergoing chemotherapy, radiation therapy, and surgery. For instance, patients with breast cancer experiencing lymphedema have shown reduced limb volume and discomfort following RLT, while those with oral mucositis from chemotherapy or radiation therapy have reported accelerated healing and reduced pain.
Mechanism of Action: The Science Behind RLT
The efficacy of Red Light Therapy (RLT) in enhancing the quality of life for cancer patients can be attributed to its fundamental mechanism, known as photobiomodulation (PBM). This process, deeply rooted in cellular biology and physiology, unlocks a cascade of beneficial effects within the body, primarily through the modulation of mitochondrial activity and the promotion of anti-inflammatory responses. Here, we delve into the scientific intricacies of RLT’s action, elucidating how this therapy works at a molecular level to support health and recovery.
THE ROLE OF MITOCHONDRIA IN PHOTOBIOMODULATION
At the heart of RLT’s mechanism of action is the mitochondrion, a cellular organelle pivotal in energy production. Mitochondria generate adenosine triphosphate (ATP), the cell’s energy currency, through a process known as oxidative phosphorylation. When red light photons penetrate the skin and underlying tissues, they are absorbed by a mitochondrial enzyme called cytochrome c oxidase. This absorption triggers an increase in mitochondrial efficiency and ATP production. Enhanced ATP availability means that cells have more energy to carry out repair processes, regenerate, and maintain their health. This is particularly significant in the context of cancer care, where cells may be damaged by the disease or its treatments.
ANTIOXIDANT EFFECTS AND REDUCTION OF OXIDATIVE STRESS
RLT also exerts antioxidant effects, helping to neutralize oxidative stress—a condition characterized by an imbalance between free radicals and antioxidants in the body. Oxidative stress can damage cells, proteins, and DNA, contributing to inflammation and disease progression. By boosting cellular antioxidant capacity, RLT helps protect cells from damage, supporting their integrity and function.
MECHANISMS BEHIND THE BENEFITS FOR CANCER PATIENTS
The clinical benefits of RLT are underpinned by its action at the cellular level, enhancing mitochondrial function, modulating inflammatory responses, and improving tissue repair and regeneration. These mechanisms contribute to the therapy’s ability to mitigate side effects, enhance recovery, and potentially exert direct anti-cancer effects through apoptosis induction in cancer cells.
ANTI-INFLAMMATORY EFFECTS AND PAIN REDUCTION
Another cornerstone of RLT’s mechanism is its ability to modulate inflammatory responses. Inflammation is a natural process involved in the body’s defense system but can become detrimental when chronic or excessive. RLT influences key pathways and signals involved in inflammation, leading to a reduction in pro-inflammatory cytokines (signaling molecules) and an increase in anti-inflammatory cytokines. This modulation helps alleviate pain, reduce swelling, and promote a more favorable environment for healing and recovery.
ENHANCING BLOOD FLOW AND TISSUE OXYGENATION
By stimulating the release of nitric oxide—a vasodilator that relaxes the inner muscles of blood vessels—RLT improves blood flow and enhances tissue oxygenation. This effect ensures that vital nutrients and oxygen are efficiently delivered to cells in need, further supporting the healing process and overall cellular function.
Despite the encouraging findings, the need for larger, randomized controlled trials remains to further validate RLT’s efficacy and optimize its application parameters. Research focusing on personalized treatment protocols, based on individual patient characteristics and specific cancer types, could pave the way for more targeted and effective use of RLT in oncology.
The current body of research and clinical evidence firmly positions RLT as a viable and beneficial adjunct in cancer care, capable of improving patient outcomes and quality of life. The endorsements from the WALT position paper and systematic reviews highlight the therapy’s potential, advocating for its broader adoption in clinical practice. As the scientific community continues to explore and understand the full spectrum of RLT’s benefits, its role in oncology is set to expand, offering new avenues for enhancing cancer care.
Potential Side Effects Mitigated by Red Light Therapy in Cancer Patients
Red Light Therapy (RLT), through its mechanism of photobiomodulation (PBM), offers a promising adjunctive approach to alleviating several side effects commonly experienced by cancer patients undergoing conventional treatments. This therapy’s unique ability to enhance cellular repair, reduce inflammation, and improve tissue health without invasive procedures makes it an ideal candidate for managing and potentially improving various treatment-related complications. Here, we explore some of the key side effects that can be positively impacted by RLT in the context of cancer care.
ORAL MUCOSITIS
Oral mucositis, a common and painful side effect of chemotherapy and radiation therapy, significantly affects patients’ quality of life by causing difficulties in eating, swallowing, and speaking. RLT has been shown to promote healing of the oral mucosa by enhancing cell proliferation and reducing inflammation, thus mitigating the severity and duration of mucositis. This can lead to improved nutritional intake and a reduced need for pain medications, contributing to a better overall treatment experience for patients.
DERMATITIS AND SKIN REACTIONS
Radiation therapy often results in dermatitis, characterized by skin redness, itching, and peeling. RLT’s anti-inflammatory properties and its ability to stimulate collagen production can aid in the repair of damaged skin tissue, alleviate dermatitis symptoms, and accelerate the healing process. By improving skin health, RLT can enhance patients’ comfort and reduce the impact of these skin reactions on their daily lives.
LYMPHEDEMA
Lymphedema, the swelling of limbs due to lymphatic system damage, is a frequent issue for patients undergoing surgery or radiation therapy for cancer. RLT can improve lymphatic flow and reduce inflammation, thereby decreasing limb volume and discomfort associated with lymphedema. This therapy offers a non-invasive option to manage swelling and enhance mobility and quality of life for affected patients.
CHEMOTHERAPY-INDUCED PERIPHERAL NEUROPATHY (CIPN)
CIPN is a debilitating side effect of certain chemotherapeutic agents, characterized by pain, numbness, and tingling in the extremities. RLT has been reported to have analgesic effects, potentially reducing neuropathic pain by improving nerve function and reducing inflammation. This can lead to significant improvements in patients’ ability to perform daily activities and overall well-being.
FATIGUE
Cancer-related fatigue is a pervasive issue that affects the majority of patients during and after treatment. While the mechanisms are not fully understood, RLT’s ability to enhance mitochondrial function and promote ATP production may contribute to a reduction in fatigue levels, helping patients regain energy and improve their functional status.
RLT presents a versatile and patient-friendly option for addressing a wide range of side effects associated with cancer treatments. Its non-invasive nature, coupled with the potential to improve patient outcomes and quality of life, underscores the value of incorporating RLT into comprehensive cancer care plans. As research continues to evolve, the scope of RLT’s applicability in oncology is expected to expand, offering new hope and improved care options for patients navigating the challenges of cancer treatment.
Red Light Therapy (RLT) stands out as a complementary modality with the potential to significantly enhance the quality of life for cancer patients. Through its foundation in photobiomodulation, RLT offers a non-invasive, low-risk approach to managing the multifaceted challenges associated with cancer and its treatments. By improving wound healing, reducing pain and fatigue, enhancing sleep quality, and aiding in the management of oral mucositis, RLT provides a holistic support system that addresses both physical and psychological aspects of patient well-being.
The scientific principles underpinning RLT—such as the enhancement of mitochondrial function, reduction of oxidative stress, and modulation of inflammatory responses—underscore its benefits in a supportive care setting. These mechanisms highlight the therapy’s capacity to foster cellular health and resilience, offering a pathway to recovery and improved quality of life that is both innovative and rooted in biological science.
As we move forward, it is essential for patients and caregivers to engage in open discussions with their healthcare teams about the integration of RLT into their care plans. The collaboration between patients, caregivers, and healthcare providers is crucial in tailoring RLT to meet individual needs and ensure its safe and effective use.
The potential of RLT in cancer care is a testament to the evolving landscape of supportive therapies that prioritize patient well-being and quality of life. By embracing RLT as part of a comprehensive care strategy, we open the door to new possibilities for comfort, recovery, and hope for cancer patients. As research continues to unfold, the role of RLT in enhancing patient outcomes and well-being will undoubtedly expand, illuminating a path toward a more supportive and holistic approach to cancer care.
References
[1] Robijns, J., Nair, R., Lodewijckx, J., Arany, P., Barasch, A., Bjordal, J. M., Bossi, P., Chillès, A., Corby, P., Epstein, J. B., Sharon, E., Fekrazad, R., Fregnani, E. R., Genot, M., Ibarra, A., Hamblin, M. R., Heiskanen, V., Hu, K., Klastersky, J., . . . Bensadoun, R. (2022). Photobiomodulation therapy in management of cancer therapy-induced side effects: WALT position paper 2022. Frontiers In Oncology, 12. https://doi.org/10.3389/fonc.2022.927685
[2] Bensadoun RJ, Epstein JB, Nair RG, Barasch A, Raber-Durlacher JE, Migliorati C, Genot-Klastersky MT, Treister N, Arany P, Lodewijckx J, Robijns J; World Association for Laser Therapy (WALT). Safety and efficacy of photobiomodulation therapy in oncology: A systematic review. Cancer Med. 2020 Nov;9(22):8279-8300. doi: 10.1002/cam4.3582. Epub 2020 Oct 26. PMID: 33107198; PMCID: PMC7666741.






